AI Isn't the Problem. ROI Is: The 2026 Affordability Reality for Healthcare Leaders
Healthcare leaders face an affordability crisis in 2026. Learn how to build operating systems that deliver measurable AI ROI, not just innovation theater.

Chet Naran
Jan 3, 2026
Healthcare leaders are entering 2026 under a different kind of pressure.
It's not just staffing shortages.
Not just regulation.
Not just the cost of care.
It's all of it… plus one fundamental shift:
Technology is no longer allowed to be "innovative." It must be affordable.
AI is moving fast, personalized medicine is expensive, and operating costs are already climbing. Leadership teams are being forced into a new reality where every investment must prove its value in measurable terms.
This isn't about adopting AI.
It's about building the operating conditions where ROI becomes inevitable.
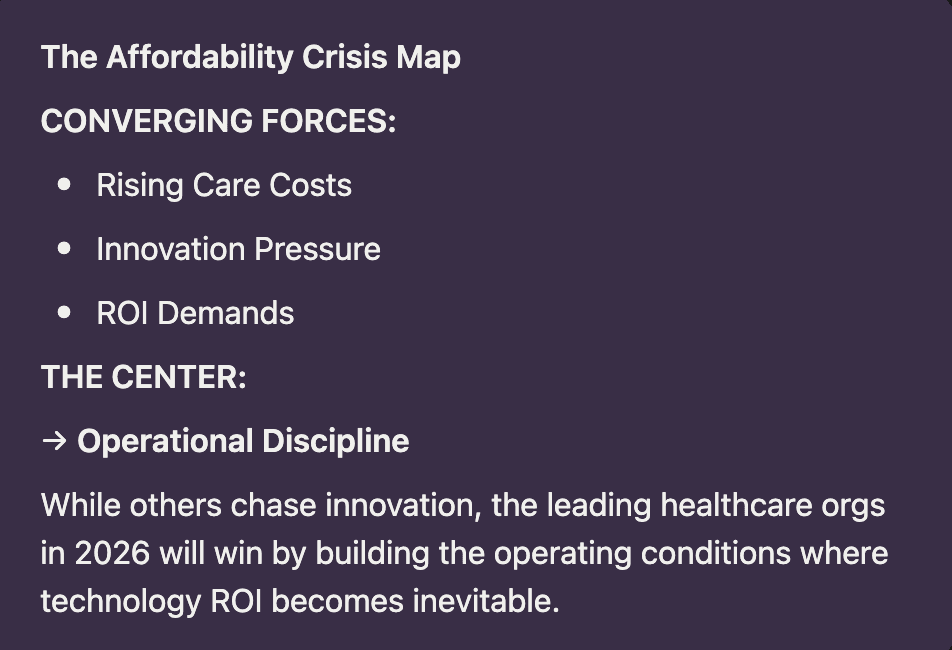
THE AFFORDABILITY CRISIS ISN'T COMING. IT'S HERE.
Healthcare is no longer operating in a "growth at any cost" era.
The industry has shifted into an affordability-first world. That changes everything about how innovation gets funded.
Leadership teams are still being asked to modernize workflows, reduce friction, and improve outcomes, but now every dollar has to justify itself with clear returns.
The most important question of 2026 isn't:
"What technology should we implement?"
It's:
"What measurable outcome will we get, and by when?"
Reflective question:
If your board demanded evidence of transformation ROI tomorrow, would your data tell a compelling story?
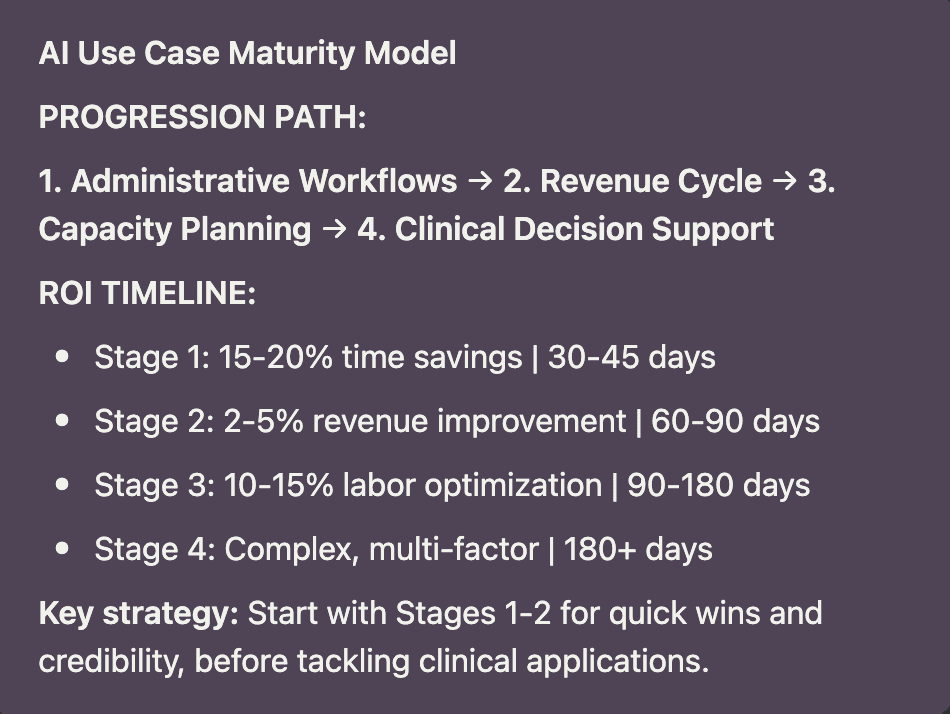
AI IS NOW INFRASTRUCTURE, NOT A PILOT
For years, AI lived in pilots, proofs-of-concept, and innovation labs.
That era is over.
AI is becoming part of core operational infrastructure, the same way cloud and EHRs did before it.
The most effective use cases aren't flashy. They're practical:
Automating repetitive administrative work
Reducing denials in revenue cycle management
Improving staffing forecasts and operational planning
Cutting down "crisis mode" workflows that drain teams
It's not that AI is getting smarter.
It's that operational leaders can't afford for it not to perform.
Reflective question:
Where in your organization could automation remove friction without compromising clinical quality or adding complexity?
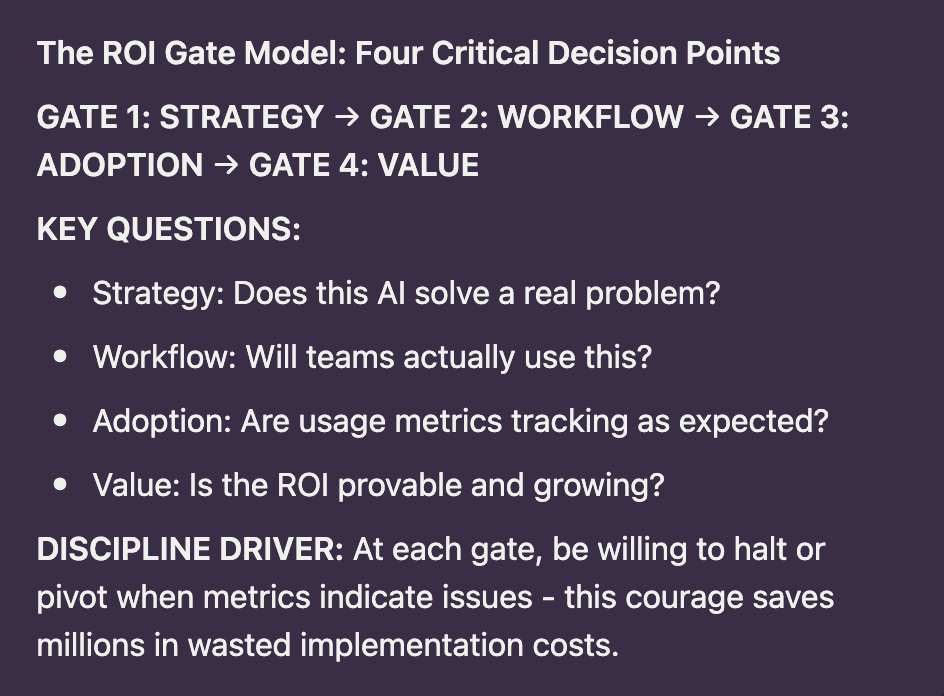
THE CFO IS NOW THE GATEKEEPER
Here's the shift most leadership teams are underestimating:
CFOs and boards aren't asking whether AI is "important."
They're asking where it's paying off and how soon.
This forces a move away from experimentation toward execution discipline.
Most organizations struggle with AI ROI not because the technology fails, but because they never establish:
A specific business case with baseline metrics
Measurable outcomes with defined timeframes
Integration into existing clinical and operational workflows
Clear accountability for adoption and utilization
The result? Expensive AI initiatives that create more noise than signal, more cost than value.
This isn't about being anti-AI.
It's about being anti-waste.
Reflective question:
If your CFO asked, "What specifically changed because of our AI investments?" would your answer be concrete or conceptual?
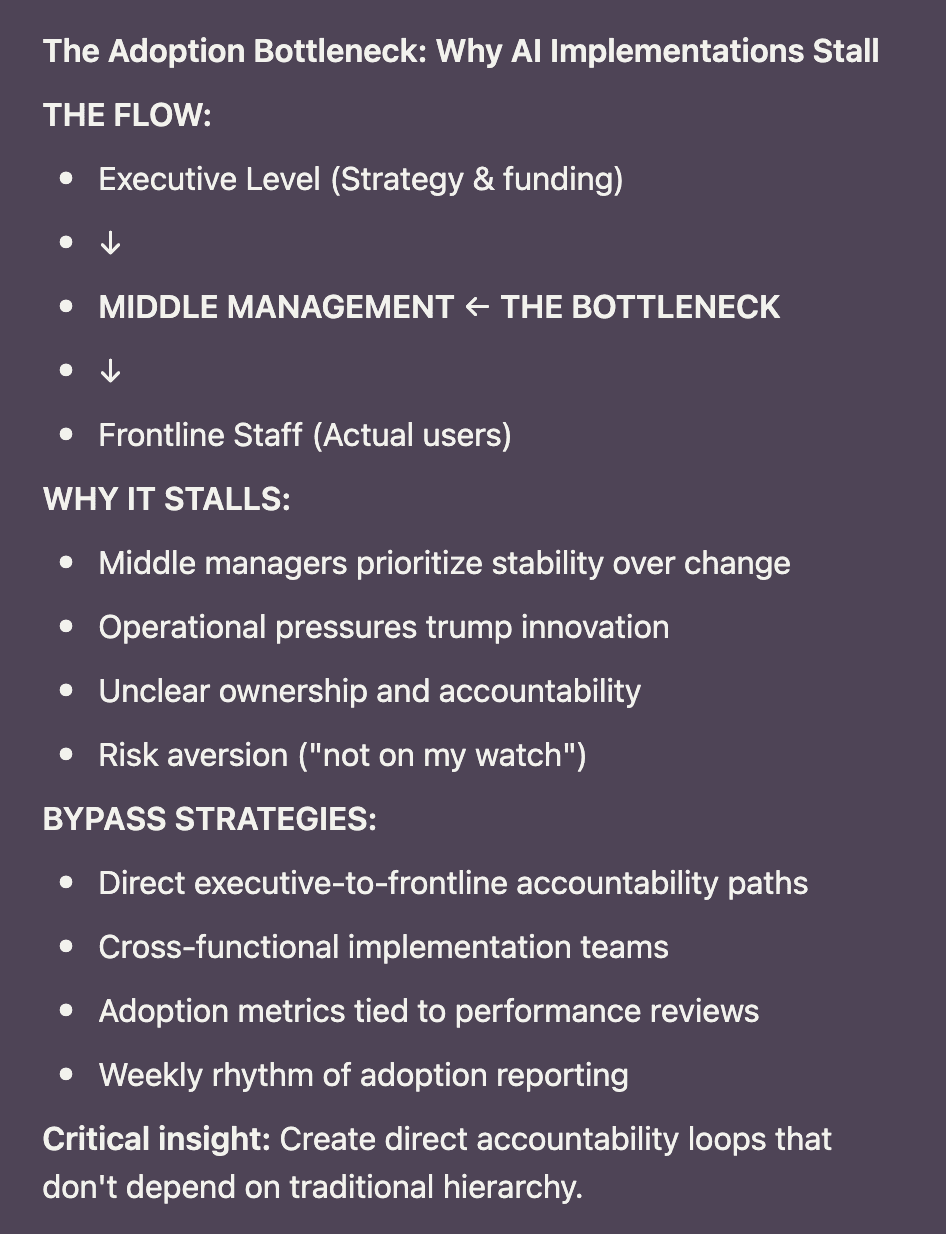
AI ROI DIES IN THE MIDDLE
Most AI investments don't fail at the executive level or the frontline.
They fail in the middle.
Middle managers protect stability because stability reduces risk in already-strained environments.
If adopting AI means changing workflows, rethinking ownership, or disrupting established routines… it often gets delayed, diluted, or quietly worked around.
So the tool gets deployed… but the organization keeps operating the way it always has.
That's precisely why ROI stalls:
Adoption remains inconsistent and optional
Workflows don't meaningfully change
Staff see AI as an added burden, not a relief
Value stays theoretical instead of practical
AI isn't blocked by technology.
It's blocked by misaligned operating rhythms and unclear accountability.
Reflective question:
Who specifically owns adoption outcomes in your organization, not just deployment timelines?
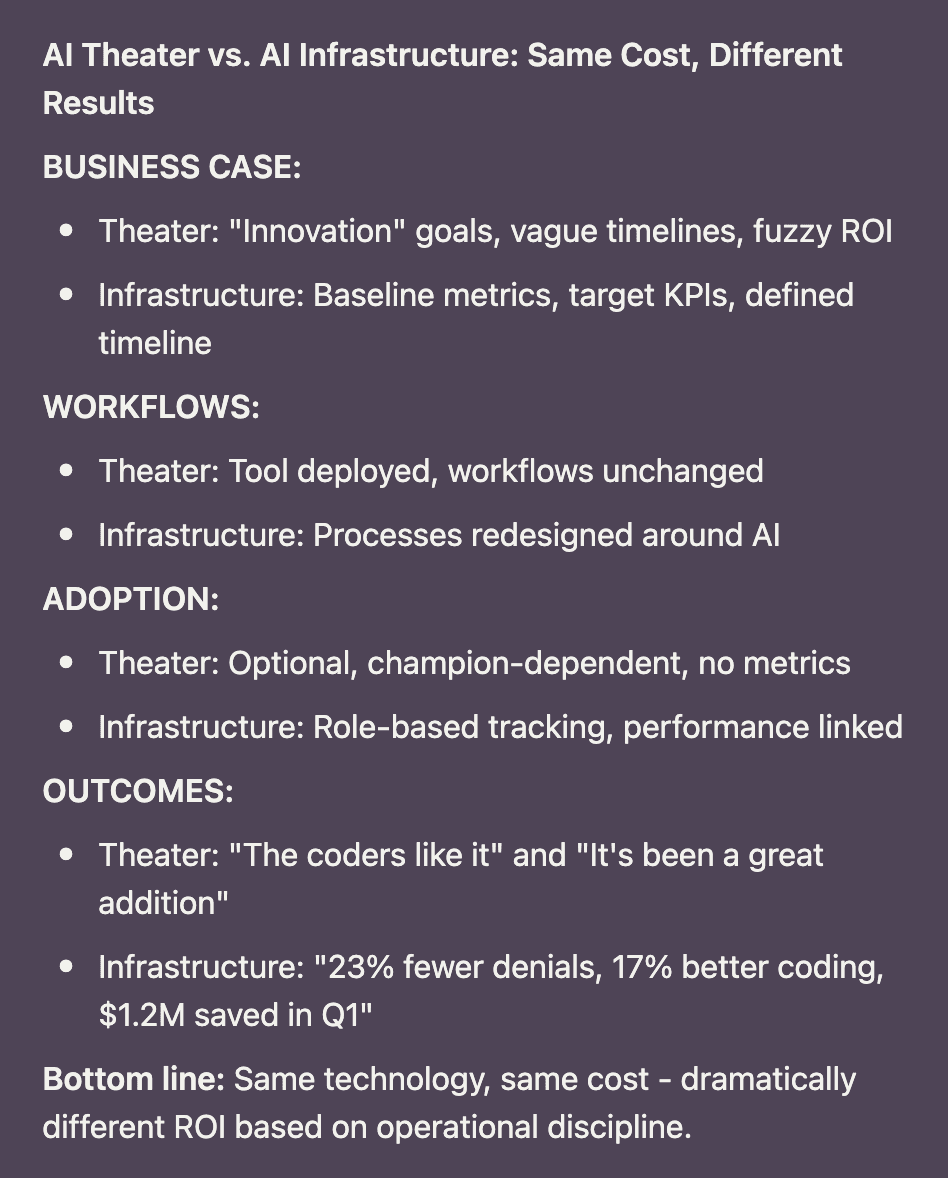
THE DIFFERENCE BETWEEN AI VALUE AND AI THEATER
You can typically tell within 60 days whether AI is becoming real infrastructure… or just expensive "innovation theater."
AI IS WORKING WHEN:
It's tied to a specific workflow with clear before/after metrics
Outcomes are reviewed weekly, not quarterly
Adoption is measured, not assumed
Leaders can trace value directly to cost reduction, throughput improvement, or risk mitigation
AI IS THEATER WHEN:
There's no concrete business case with baseline data
Workflows remain fundamentally unchanged
Results are described in anecdotes, not metrics
Utilization depends on a few internal "champions" rather than standard process
The difference isn't the technology.
It's the operational discipline surrounding it.
Reflective question:
Are you measuring AI adoption with the same rigor you measure financial performance?
HUMAN MOMENT
It's the business version of buying a treadmill in January and being shocked when it doesn't automatically improve your fitness by March.
VENDOR-POSITIVE CALLOUT
Let's be clear: excellent vendors exist.
There are outstanding AI platforms, analytics tools, and operational systems available to healthcare organizations.
The issue is rarely the vendor's technology.
The issue is whether the leadership team has:
Aligned the investment to specific operational outcomes
Created the right implementation and adoption rhythm
Built the conditions for sustainable utilization
Established a consistent value measurement framework
Technology can accelerate transformation.
But it can't replace operational leadership and implementation discipline.
FOOD FOR THOUGHT
2026 will reward healthcare organizations that treat AI like infrastructure and treat ROI as a leadership responsibility, not a vendor promise.
The winners won't be the teams that chase every new tool.
They'll be the teams that modernize their operational foundation:
Governance that scales without slowing decisions
Workflows that reduce friction rather than adding it
Adoption that becomes standard practice, not an exception
Metrics that tell the truth about both utilization and impact
You don't need more disruption.
You need operational direction.
FINAL QUESTION
As you head into 2026, which deserves your strategic investment: another AI pilot, or finally building the operating system that turns technology into measurable outcomes?