Interoperability Isn’t a Technology Problem. It’s a Trust Problem.
What healthcare leaders should ask before they invest in another integration, platform, or AI initiative.

Chet Naran
Jan 9, 2026
Interoperability has been a headline in healthcare for years.
But in 2026, it’s not just a technical initiative anymore.
It’s turning into a leadership reality check.
Because healthcare organizations aren’t just trying to exchange data.
They’re trying to make decisions faster.
They’re trying to reduce friction.
They’re trying to scale value-based care, automation, and AI, without breaking the teams that deliver care.
And when interoperability breaks, it doesn’t just cost time; it costs trust, margin, and clinical confidence.
That’s the part that’s hard to explain until you’ve lived through it.
When data stops flowing cleanly, people don’t stop working. They just start compensating.
And in that world, the real question isn’t:
“Can we connect systems?”
It’s:
“Can we trust what we’re seeing… and can our teams use it when it matters?”
This isn’t about APIs or standards.
It’s about trust, in the data, in the workflow, and in the organization’s ability to govern both.
The Real Definition of Interoperability (In Practice)
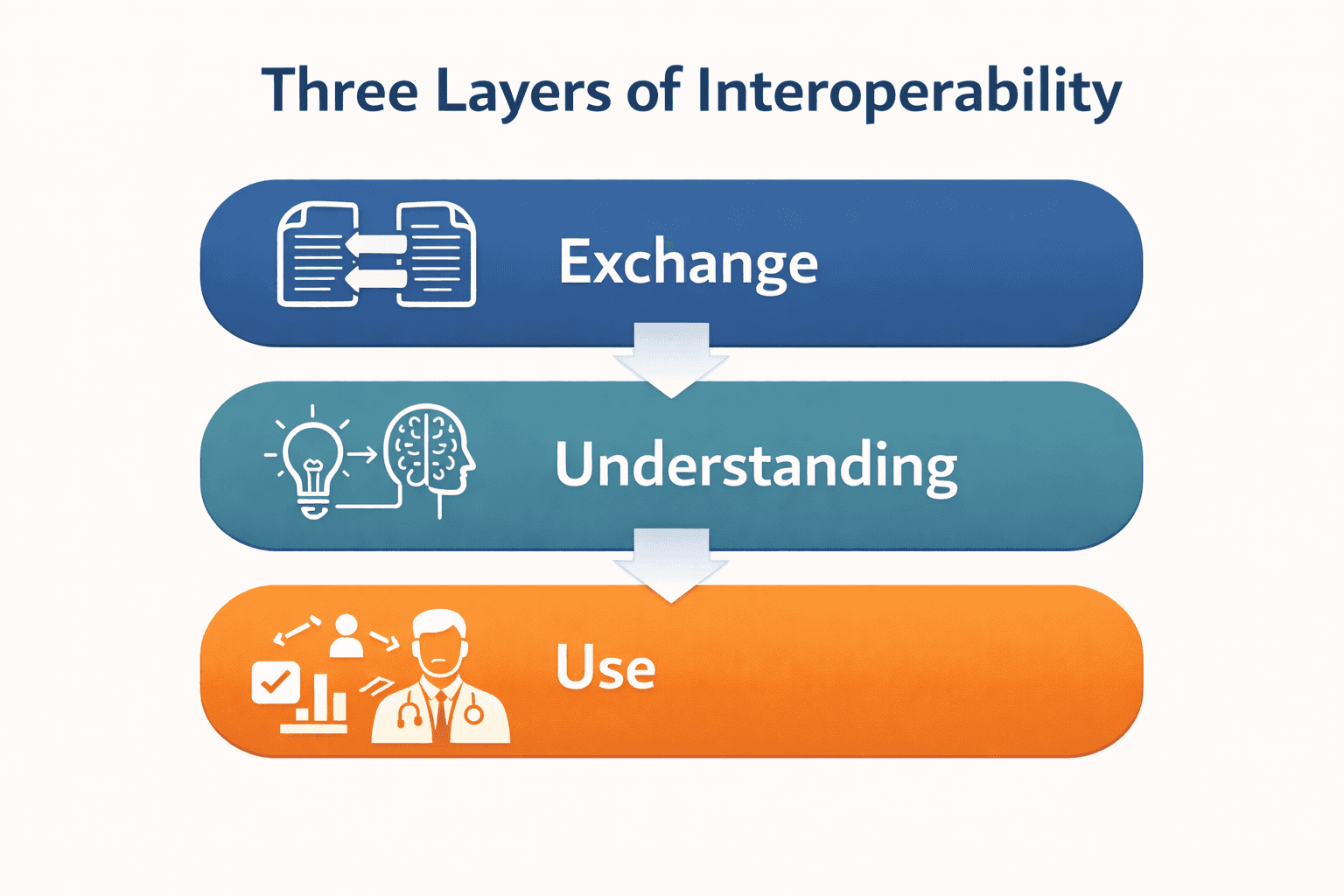
Interoperability is often reduced to “data exchange.”
But most healthcare leaders have learned the hard way:
Data moving doesn’t mean anything improves.
Real interoperability means a healthcare organization can:
Exchange data and send it somewhere
Understand the data and interpret it consistently
Use the data and apply it inside real workflows without extra burden
Most organizations can do #1.
Many can do #2 with effort.
Very few have mastered #3.
And that’s where trust either forms… or breaks.
Reflective question:
If your board asked tomorrow whether “interoperability” is improving performance, would you have a confident answer, or a technical explanation?
Where Interoperability Breaks: The 4:30pm Moment
Interoperability rarely breaks during a demo.
Or in a planning deck.
Or in a vendor roadmap session.
It breaks at 4:30pm on a Thursday.
When the day is heavy.
The clinic is behind.
The team is tired.
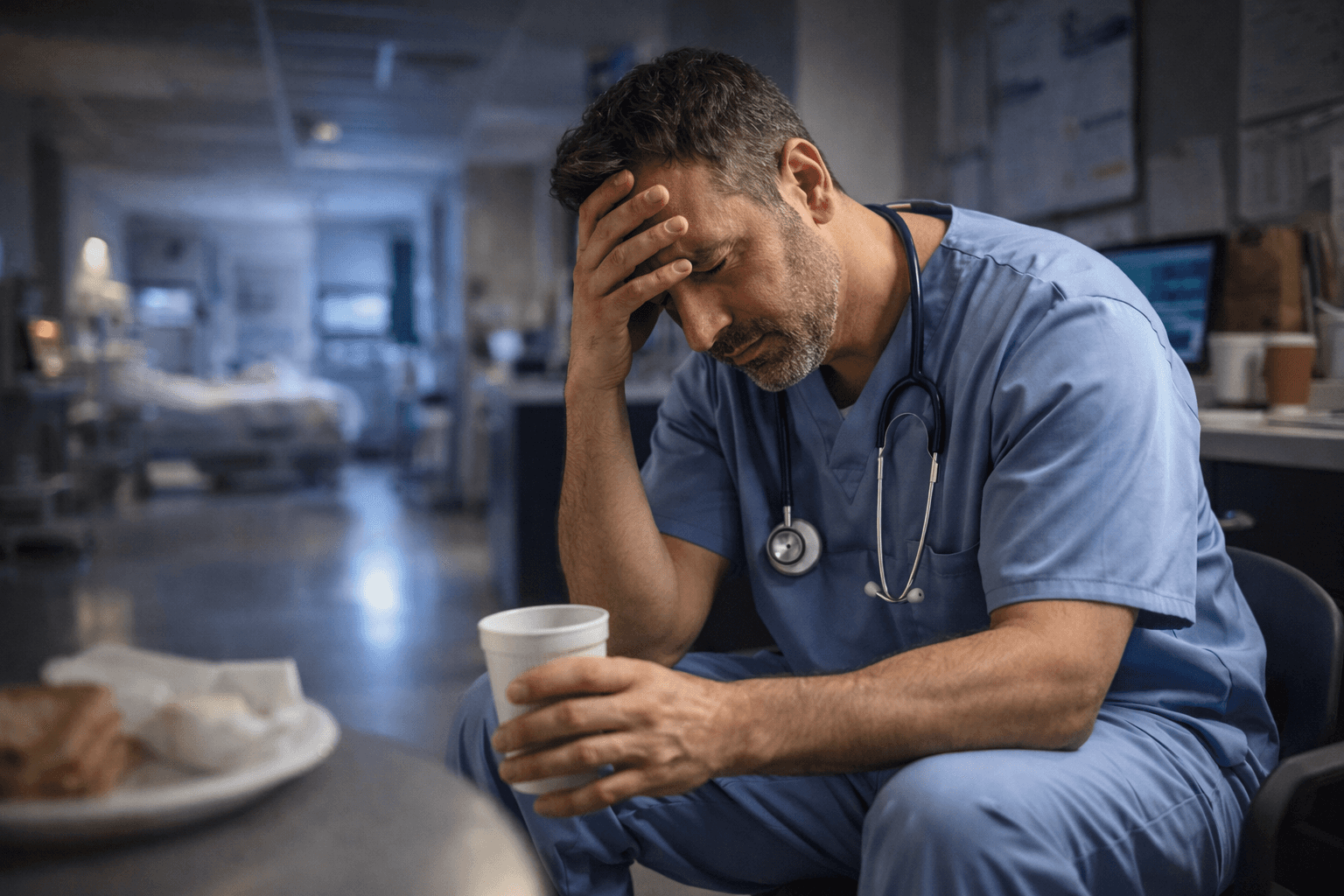
That’s when the operational truth shows up:
A referral arrives… but the receiving team doesn’t trust what they see
A discharge summary is available… but no one knows where it lives in the workflow
A lab result is in the system… but it’s missing context
A patient gets asked the same question twice
Someone says: “Just to confirm…” for the fifth time today
That “just checking” energy?
It’s not a personality issue.
It’s a visibility and trust issue.
Interoperability breaks when the system stops carrying the work, and people start carrying it in their heads.
Two Real-World Patterns (Anonymized)
Example 1: “We Have the Data… But No One Uses It”
A growing healthcare organization had built extensive interfaces between systems.
Technically, data was flowing.
But clinicians weren’t using outside records because:
The info landed in a separate tab
It wasn’t normalized
It required extra effort to interpret
and it wasn’t trusted under pressure
In leadership meetings, interoperability was considered “complete.”
In practice, it was invisible.
The result: more duplicated work, more clinical friction, and no improvement in care coordination.
Example 2: “The Integration Works… Until the Workflow Doesn’t”
Another organization implemented a connectivity solution to unify billing and clinical events.
The integration worked.
But nobody clarified:
Who owned errors
Who was accountable for monitoring
What “done” meant operationally
or how teams would adjust when exceptions occurred
So, when a downstream break happened, it took weeks to pinpoint ownership.
The technology didn’t fail.
The operating conditions did.
The Hard Truth: Interoperability Isn’t Mostly Technical
Here’s the uncomfortable reality most teams eventually face:
Interoperability isn’t primarily a technology challenge.
It’s a governance + incentives challenge disguised as a tech project.
Hospitals compete.
Payers compete.
Vendors compete.
Teams protect their workflows.
Data becomes power.
And power rarely moves freely without clear agreements.
Which means interoperability isn’t just “integration work.”
It’s organizational maturity.
Reflective question:
Do you have an interoperability strategy… or just a series of integration projects?
What Leaders Should Ask Before Buying Another Solution
Before investing in “interoperability platforms,” “FHIR tools,” or “AI-driven automation,” it helps to ask:
1) What is interoperability for?
Care coordination? Patient access? Analytics? AI readiness? Value-based care? RCM performance?
Because interoperability without purpose is expensive plumbing.
2) What is your “source of truth” for identity?
If patient matching and provider identity are inconsistent, everything else becomes fragile.
3) Are you exchanging documents… or data?
Documents move information.
Structured data enables action.
4) Does outside data land inside workflow?
Or does it land “somewhere” that nobody touches?
5) Who owns adoption?
Because exchange isn’t the finish line.
Utilization is.
AI Isn’t the Enemy Here, it’s the Accelerator
AI is often framed as the force that will “solve interoperability.”
That’s not quite true.
AI doesn’t eliminate the need for accurate data, clear ownership, or trusted workflows.
But it does change the equation in a different way.
The future isn’t AI replacing interoperability, it’s AI accelerating the work that humans can’t scale.
Because AI can provide the automated labor needed to turn fragmented, inconsistent, messy operational data into something usable.
In healthcare, that acceleration only matters if the guardrails are real: patient safety, oversight, and privacy-by-design.
In other words:
AI isn’t just a consumer of clean data.
It can be part of the engine that creates it.
Where interoperability efforts used to take months of manual mapping, cleansing, reconciliation, and standardization, AI can reduce that time dramatically by supporting:
Entity matching and deduplication (patients, providers, locations)
Code normalization across vocabularies (LOINC, SNOMED, RxNorm)
Data classification and quality checks at scale
Workflow automation that reduces handoff friction
Pattern detection that reveals where trust breaks down in flow
That doesn’t mean the problem is solved.
It means the work becomes more possible, if the organization has the discipline to guide it.
The real question isn’t whether AI can help.
It’s whether leadership teams are ready to direct AI toward operational clarity instead of novelty.
Because when AI is deployed with the right guardrails, it becomes less about hype… and more about building trust in the ecosystem.
AI doesn’t replace interoperability.
But it can accelerate the work of making it real, if governance and workflows are clear enough to support it.
Vendor-Positive Callout (Required)
Let’s be clear: excellent vendors exist.
There are outstanding interoperability platforms, integration partners, and tools available to healthcare organizations today.
But interoperability success rarely comes down to the vendor.
It comes down to whether leadership has:
Aligned the effort to operational outcomes
Clarified governance and ownership
Designed workflows that use data without burden
Established measurement and accountability rhythms
Created a shared truth the organization trusts under pressure
Technology can accelerate transformation.
But it cannot replace leadership discipline.
The First Practical Step (Without Starting a Huge Project)
If you’re not sure where to begin, start here:
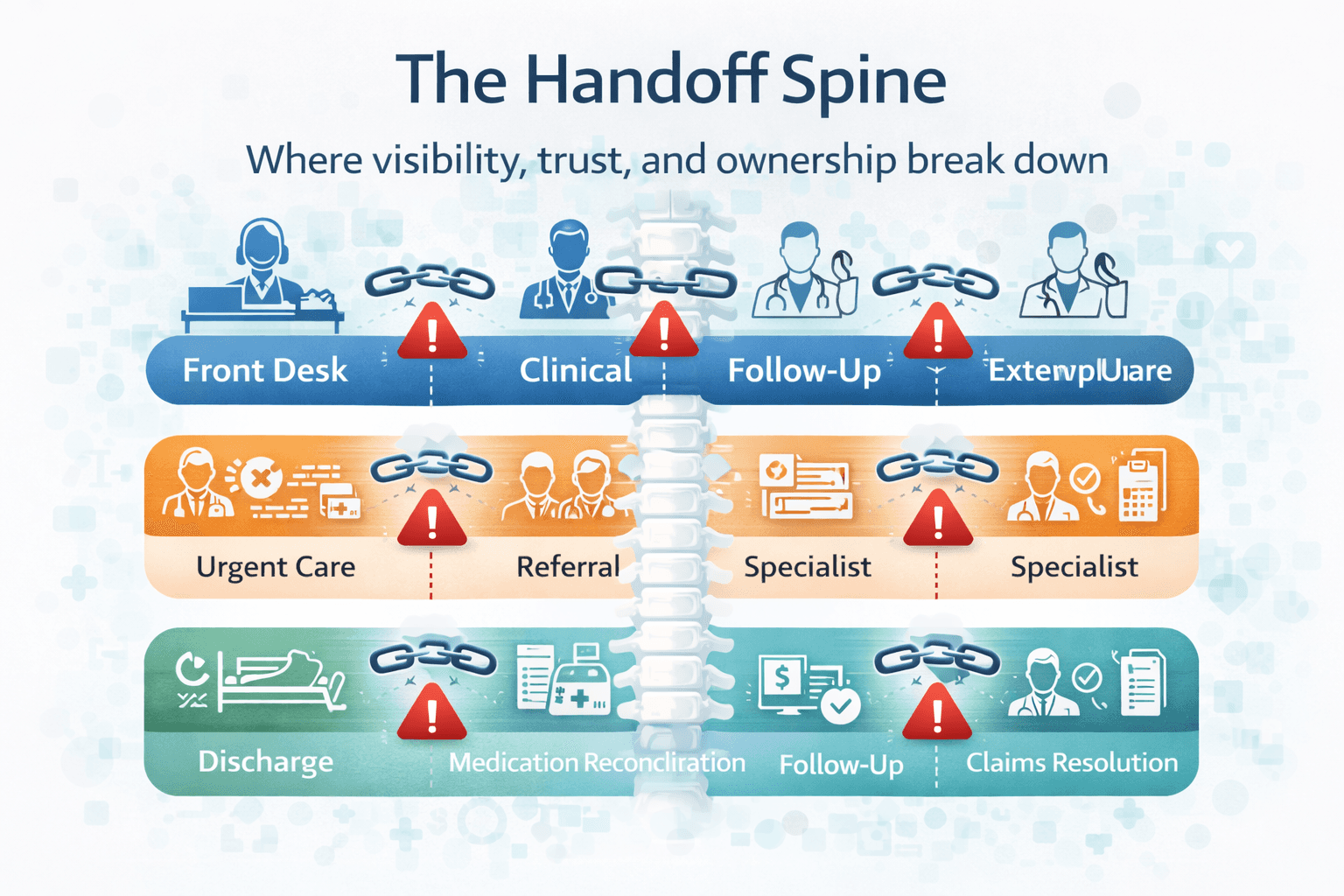
Map one high-friction handoff flow.
Pick one operational chain where breakdowns create friction, for example:
Front desk to clinical to follow-up
Urgent care to referral to specialist
Discharge to medication reconciliation to follow-up
Clinical documentation to billing to claims resolution
Then ask three questions:
Where does visibility break first?
Where does trust break first?
Where does ownership become unclear?
You don’t need to solve everything.
You need a clear “handoff spine”: a simple backbone that makes work visible and reliable, even on hectic days.
Bringing this home (Present to Future)
2026 won’t reward organizations that build the most integrations.
It will reward organizations that build operational trust:
Systems people believe
Workflows that reduce burden
Governance that scales
Data that becomes a reliable input, not a liability
Interoperability will increasingly define:
Patient experience
Provider satisfaction
Revenue performance
AI readiness
and the ability to scale without burnout
Not because healthcare needs more technology.
But because healthcare needs more confidence in how it operates.
A Final Question
As you head deeper into 2026, are you investing in another tool to exchange data…
or are you building the operational trust that makes interoperability real?